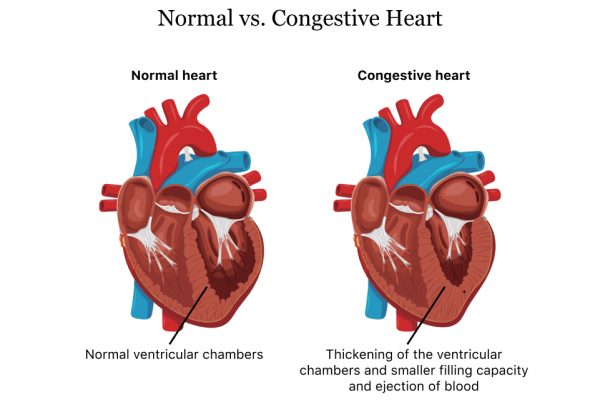
Chronic medical conditions are persistent, long-term disorders that require frequent care to improve patient health and comfort. Chronic conditions, which include Alzheimer’s disease, cancer, diabetes, depression, and rheumatoid arthritis, are the leading causes of disability and death—they affect about 60 percent of Americans. Moreover, medical care and management of these conditions accounts for roughly 90 percent of the United States’ $4.1 trillion in annual health care spending.
Chronic care management (CCM) is a relatively new preventative care paradigm, introduced about a decade ago, that helps providers deliver effective comprehensive care plans to patients with two or more chronic conditions, an issue that affects more than 40 percent of Americans. Patient benefits include coordinated services, such as ongoing support and education, and lower risk of hospitalizations and emergency department visits. Specific services include prescription refills, symptom management, preventative health counseling, and social support. CCM services are covered in Medicare Part B.
CCM can be even more successful when combined with remote patient monitoring (RPM) technology. Many healthcare organizations, including TapestryHealth, led by CEO Mark Hirschhorn, offer innovative tech-focused solutions to more effectively manage chronic conditions. Below is a review of RPM and its potential to improve healthcare outcomes when used to complement CCM.
What is remote patient monitoring (RPM)?
While it isn’t a new practice, providers increasingly turned to RPM during the COVID-19 pandemic in efforts to remotely treat patients. Providers are continuing to utilize RPM technology, including wearable connected devices, to track patient vital signs and other physiologic data that informs critical physician decisions. RPM devices can monitor blood pressure, heart rate, and the amount of oxygen in the blood, among other numerous other health metrics and vital signs. Data is continuously collected and transferred electronically to providers, often in real time, in easy-to-read graphs and reports. Physicians can then use this data to inform treatment options based on the patient’s condition, lifestyle behaviors, and medications.
How can RPM complement CCM?
RPM simply gives providers more information to make important medical decisions—it enables a preventative approach to health care as opposed to reactionary. For example, if an RPM device notices irregularities in a patient’s vitals after a prescription change, a physician can look at the real-time insights to make the necessary adjustments. These and other digital health innovations, including AI-enabled insights and telehealth, also allow patients to take a more active role in managing their health. This is especially important for people in rural areas, people in post-acute facilities, and anyone without the ability to visit their physician on a regular basis.
Why doesn’t every healthcare facility offer RPM?
Advances in technology, increasing caseloads at hospitals, and Medicare reimbursement has led many providers to begin offering RPM as a means of tracking the health of patients with chronic conditions. However, a lot of providers are still hesitant to change the way in which they treat and communicate with patients. While RPM claims increased fourfold from January 1, 2019, to March 31, 2021, fewer than 1 percent of all physicians accounted for those claims.
A lot of the hesitancy among providers to adopt RPM can be attributed to overburdened practices and clinicians being uncomfortable altering their method of health care delivery. Yet, providers can bill for both RPM and CCM and work with an organization specializing in remote care technology, such as TapestryHealth, to implement these programs. Moreover, RPM and CCM do not replace in-person care, but provide physicians with critical information to make informed treatment decisions, leading to better patient outcomes.
What are some examples of RPM platforms?
TapestryHealth, led by CEO Mark Hirschhorn, is multi-specialty healthcare company that champions the value of RPM, especially as a way to more effectively serve patients with two or more chronic conditions. The company provides solutions for skilled nursing facilities and other post-acute environments. Through a partnership with electronic health records (EHR) provider Rosie Connectivity Solutions, Tapestry offers its RPM solutions, including its Vitals Management Program, to hundreds of facilities in more than 35 states. Additionally, Tapestry’s AI data and analytics solutions help facilities mitigate risk and reduce rehospitalizations by predicting patient declines and adverse health events. The company is also a major proponent of further RPM adoption in skilled nursing facilities.
“We want to bring more attention to the fact that there needs to be greater collaboration with the payers and with those facilities that can feel a bit more emboldened to ensure they can create a greater care setting,” Mark Hirschhorn said in a 2022 interview with Skilled Nursing News. “If this is sponsored at a national level, we believe that there will be a greater opportunity to provide services along with the payers (in our case Medicaid and Medicare) [which will] lower cost overall, and address issues at the point of care, as opposed to having greater costs down the road.”