It is essential in healthcare that everyone receives equal treatment, no matter who they are, where they are from, and what they do. Sadly, however, specific groups of people tend to find more difficulty getting the healthcare they need than most.
These people often make up ‘vulnerable populations’. But what makes these populations so vulnerable, and how can healthcare providers support them better?
Medical care can be complex and, for many people, difficult to find. Thankfully, individual nurses can make a difference to patients in the fight against healthcare inequality.
Let’s take a closer look at what ‘vulnerable’ means in this context, who certain groups might include, and how healthcare providers can improve their access to support.
What are vulnerable populations?
In healthcare, we can define vulnerable populations as those at a greater risk of poor health. They are also at risk of having poor access to healthcare. Vulnerable populations are generally more likely to experience unfair treatment in healthcare organizations. However, this is a generalization, so it’s important to look closely at the types of people who may feel unsupported.
As time goes on, it appears that these populations are growing in numbers, causing devastation for wider healthcare and millions of people across the US (and abroad).
With this in mind, why are vulnerable populations so important to the healthcare system in general?
Why are vulnerable populations important?
Due to the unfair disparity between vulnerable populations and those who are not, people in vulnerable groups are far more likely to develop severe medical issues that will go untreated or receive poor levels of care.
This can quickly lead to a higher mortality rate in specific groups and areas, an increase in the contagion of diseases, and even more significant issues down the line.
Sadly, the number of vulnerable populations appears to be increasing, not decreasing. This is partly due to the longevity of life in many people increasing and poverty gaps widening, among other problems.
With the number of vulnerable populations and untreated patients growing, it is vital to pass our focus on to these groups. Ensuring that they get the care they need and deserve is of the utmost importance for these populations, the healthcare system, and the country.
But how can you identify people of vulnerable populations? Is it easy to avoid making generalizations, and how do healthcare providers strike this balance?
How healthcare providers determine vulnerabilities
People of vulnerable populations are determined based on multiple factors. What often comes into play includes their age, race, sexuality, socio-economic status, location, and current health status. They are also judged based on cultural factors, however unfair and biased they may be.
One person can also have multiple factors ‘working against them’ regarding their desire for healthcare. For example, you could be both elderly and part of the LGBTQ+ community, making it increasingly more difficult for you to get the healthcare you need in some cases. It’s simply unfair that people in these groups receive poor care standards, especially when they have no control over their circumstances.
Types of vulnerable populations
In healthcare, the following vulnerable populations are frequently analyzed and discussed. Regrettably, many face discrimination, and while healthcare workers should always follow a firm code of ethics, people in these groups face marginalization and struggle to get the help they need.
Let’s take a look at who may face the most impacts of all.
People on low income
Low-income people are proven to receive unfair treatment when it comes to healthcare access.
As we all know, healthcare can be costly, especially in the US. Getting access to health insurance can also be very difficult. Where you are from, your current income, your job, and your career path can all affect how you access healthcare on a purely monetary basis.
Low-income people often find that they are at the back of the queue for healthcare due to a lack of finances. They are not seen as able to afford the healthcare and treatment they need, so they no longer receive priority treatment.
This means that low-income people are more likely to have chronic diseases and are far more likely to go untreated (or receive poor care).
It also means that people on a low income are less likely to seek out help when needed, out of fear of rejection or of being faced with high medical costs.
The homeless
Along with low-income populations, the homeless are also less likely to gain access to the healthcare they need. They face the same issues as low-income populations: they do not have access to health insurance. However, their problems can arise from more than that alone.
As homeless people, they are less likely to have access to basic commodities, even to access the medical centers they need to visit. And should they need ongoing treatment, they may not be able to find anywhere safe to stay as they receive care.
In some cases, certain healthcare workers may refuse to help homeless people with substance abuse problems (as an example). Some people suffering from withdrawal may be violent or unpredictable, which can lead to pigeonholing.
Refusing care based on background and appearance is unethical. However, in many cases, homeless people can find themselves against the odds of getting the medical support they deserve.
Homeless people are at a much higher risk of getting diseases or chronic health issues. It’s also worth remembering that ‘homeless’ isn’t a blanket term that purely applies to people living on the streets and/or people who may be addicted to drugs and alcohol. This is a highly complex and marginalized group.
Disabled people
Disabled individuals are far more likely to need multiple and even frequent interactions with the healthcare system than those who are not.
However, due to their disabilities, they may have difficulty accessing the care they need. This can be due to reduced mobility, lack of physical access to the buildings in question, the expense of the care they need, and general judgment from the healthcare practitioners they know.
It’s important for healthcare providers and clinics to ensure that they provide services as accessible as possible to a wide range of physical and mental disabilities (or ‘invisible conditions’).
People with chronic illness
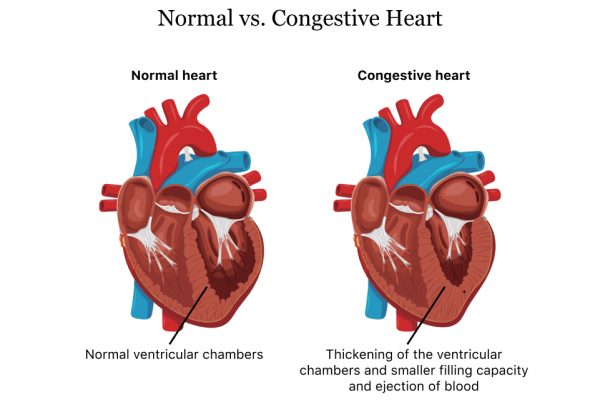
Similarly to disabled individuals, patients with chronic illnesses are certain to have far more interactions with the healthcare system than those without chronic disease.
This means much higher and far more healthcare bills and having to deal with multiple healthcare providers, even at once.
Therefore, people with chronic illness have proven to have more poor health days and poorer interactions with the healthcare system than the general population on average. This, unfortunately, means that they’re a vulnerable population as far as the definition stretches.
Poor communities
Low-income groups do not always refer to families or individuals. Indeed, entire communities can have difficulty getting access to quality healthcare.
Poorer communities are often made up of specific racial groups due to racial inequality within their region, as well as a disproportionate distribution of wealth.
This means that in some areas of the US, people of African-American or Hispanic descent are far more likely to encounter issues when seeking out healthcare. This can include getting access to health insurance, reaching reputable healthcare organizations, or even being prioritized when necessary due to discrimination.
Certain geographical areas
Sometimes, simply being in ‘the wrong location’ is enough to ensure that you do not get the healthcare you need. This is simply due to isolation or a significant distance from highly populated areas.
For example, those living in New York City are far more likely to have access to all kinds of medical professionals, equipment and treatment than those living in a small rural area, far from the hustle and bustle of the big cities.
Therefore, to get the medical treatment they need, there is the added expense of travel, staying in the area during the treatment, etc. This means that many will not be able to get the treatment they need simply due to the expense and hassle of not being in the best area for their medical needs. Once again, this isn’t always the fault of the people impacted.
Young people
Young people, specifically children, are far more vulnerable to disease and viral spread than most. Regrettably, pediatric care remains somewhat underfunded, putting young people at a significant disadvantage.
In some cases, children are often treated as ‘small adults’ regarding their care – in the sense that they are not always prioritized based on their age or vulnerability. This means that they are not given adequate care, which can lead to further issues or worse.
Children also lack the autonomy to make their own decisions based on factual information – they are not always able to understand their current health status.
Therefore, this responsibility falls to the parents or guardians. While there are systems in place to help protect the children’s best interests, this naturally sets them more at risk than adults who can make their own decisions.
Young people may not always get the care they need if parents or guardians are unwilling to support them. Social care therefore aims to ensure that children’s health receives the priority it deserves.
The elderly
Elderly people make up another group of people who are more at risk of getting diseases, illnesses and injuries than most. Therefore, they rely on healthcare organizations often far more than the general adult population. They have lower immune systems and generally weaker bodies. Of course, this leads to higher and more frequent medical bills. However, their vulnerabilities do not start and end here.
Making their way to their medical appointments can be a challenge, as can their at-home care and generally abiding by the doctors’ recommendations. Without being appropriately followed, the elderly are far more likely to succumb to their ailments, which, sadly, has proven to be the case more often than not.
The elderly population was a central healthcare focus at the height of the COVID-19 pandemic, through which people over the age of 65 were some of the most sensitive to the emerging coronavirus. Poor handling of the virus in some regions led to many unnecessary elderly fatalities – for example, in residential homes that failed to lock down appropriately.
LGBTQ+
People of the LGBTQ+ community have proven to be confronted with far more discrimination than the general public when it comes to healthcare. Therefore, this has led to a large number of the LGBTQ+ community avoiding seeking healthcare when needed out of fear of discrimination.
There is also a significant disparity within the LGBTQ+ community. For example, an African-American transgender woman is far more likely to miss out on quality healthcare than a homosexual white woman.
People in the LGBTQ+ community are more likely to need medical help, especially when it comes to mental conditions. In fact, people in the LGBTQ+ community have a higher suicide and depression rate than those who are not in the community.
How can healthcare support vulnerable populations?
There are multiple ways that the healthcare system can help vulnerable populations. However, it is essential to locate the issues and their sources correctly to be able to address them.
One way that the healthcare system can help support vulnerable populations is by providing help and support for those who cannot afford healthcare. This can be due to a lack of employment, a home, or even communal issues such as illiteracy, food disparity, or otherwise.
Another example of how the healthcare system can help vulnerable populations is by investing more time in virtual healthcare. During the height of the COVID-19 pandemic and consequential lockdowns, millions of people across the globe had to interact with their healthcare specialists from afar, using tools such as Skype, Zoom, FaceTime, and even email.
This proved beneficial and allowed more patients to be seen and heard. While it is vital to see your doctor in person to get the best treatment possible for specific issues, talking with them directly can be enough and can save transport and time.
It’s also crucial for medical care teams to remember their ethical codes of practice. While providing healthcare as it stands is enough to satisfy treatment requirements and ‘tick boxes’, there are still some cases where ethics are ignored from scenario to scenario.
Nurses and doctors should, for example, always treat patients based on specific care needs and never on superficial determiners. It is grossly unfair to provide a lower standard of care to a patient based on their appearance or living standards, for example. Unfortunately, there are still cases where people face marginalization for factors beyond their control.
Creating better links between rural community health centers and hospitals is also essential. Providing the necessary treatment to those in need means reducing the effects of geo-isolation. This would allow for a more accessible healthcare standard across the nation for all groups involved, no matter how isolated they may be geographically.
Finally, a big way that the healthcare system must address vulnerable populations is by addressing the overall cost of healthcare. Healthcare costs, especially in the US, can be absolutely bankrupting.
Focusing on a new way of funding the healthcare system (including research, education, practice and aftercare) that allows people everywhere to prioritize their health and wellbeing without having to worry about the cost could make all the difference in the world.
What can individuals do?
Unfortunately, expecting seismic shifts in the US medical system is unwise at this time. It’s highly complex, and untangling the cost aspects of healthcare could take years of legal wrangling. It’s not impossible, of course, to see change – as the so-called ‘Obamacare’ provisions suggested several years ago.
However, nurses and other practitioners must do what they can to provide a fair and accessible service to all. Starting by enrolling on an accelerated nursing program online, such as via Elmhurst University, nurses can quickly learn how to make ethical practice the core of what they do.
Ethically minded and motivated individuals can, together, help to make clinics and healthcare services more accessible and more reliable for all, regardless of vulnerability or group. It may take time, but it is the least that the individual can do, regardless of territory or role.
Conclusion
As you can see, there is no shortage of vulnerable populations in healthcare in the US. As much as we live in a technologically advanced country, our healthcare system still has a long way to go. For so many groups, simply having access to healthcare seems impossible – be it due to their financial state, race or sexual orientation. For such a proud and capable country, this should not be the norm.
Thankfully, the healthcare system is always looking for new ways to help the general population and each individual in whatever form it can. A healthy system can only operate so well on the talent and strength of the doctors and nurses who keep it running.
Hopefully, in the years to come, marginalization and vulnerable population classifications will slowly dissipate, and we can all expect the same level of care.